65 year old male Libyan patient, known case of HTN (1 year) off ttt, presented with chest pain and palpitations
- Chest pain is new onset
- Past history of palpitations a few months back
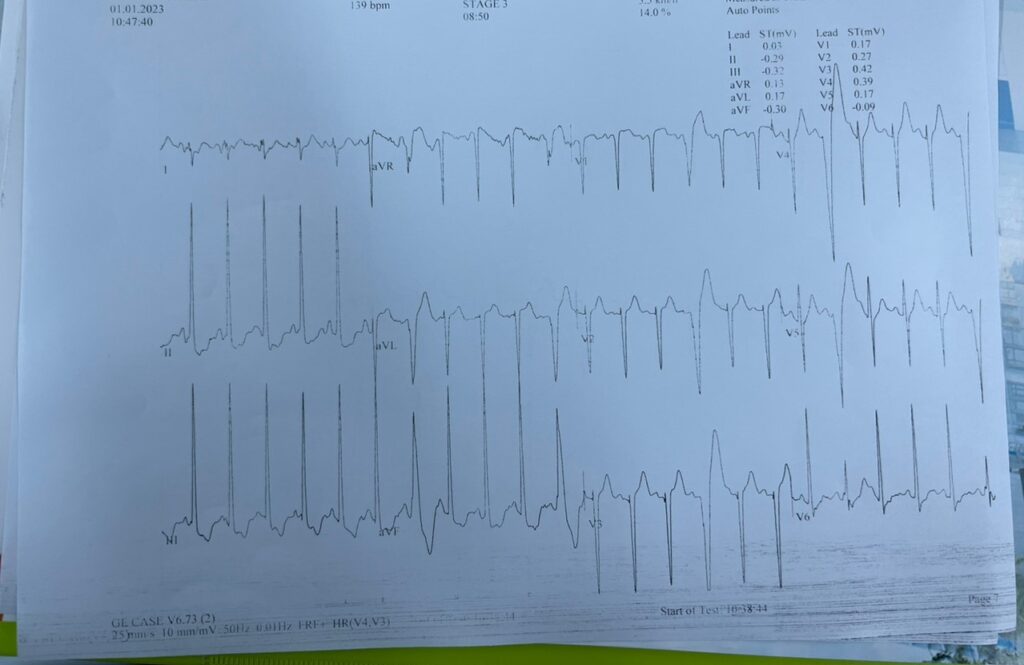
This was his ECG on presentation
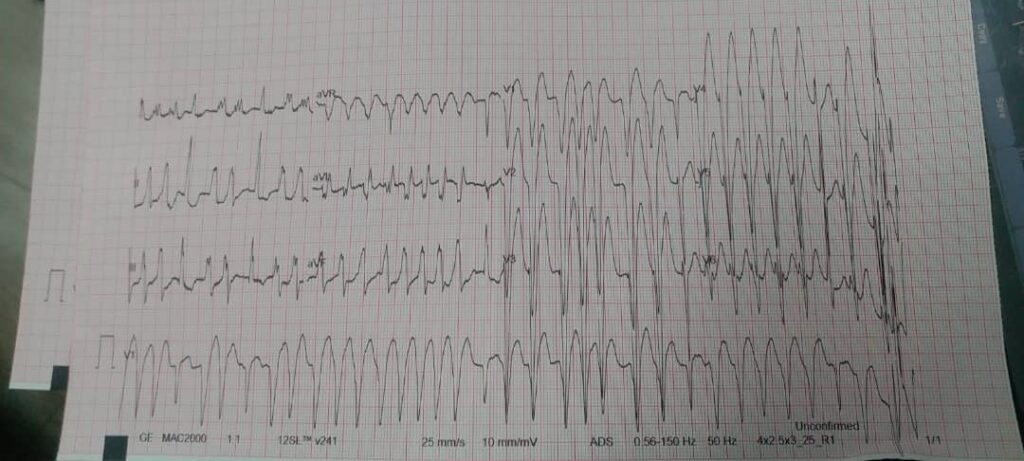
On first glance this rhythm strip crosses most of the ECG criteria for VTACH, so the DOD went with the assumption that this could be a polymorphic VTACH
They started chemical cardioversion with 150mg Cordarone twice, but there was no response, and as the patient started getting a little drowsy, the doctor took the decision to initiate thrombolytic therapy, as they suspected that the cause of this arrhythmia could be an underlying ischemia.
Cardiac markers and a full metabolic panel were sent during the management of the patient.
DC shock was also commenced after checking that the patient’s BP was recordable, and right after the electrical cardioversion the patient reverted to sinus rhythm.
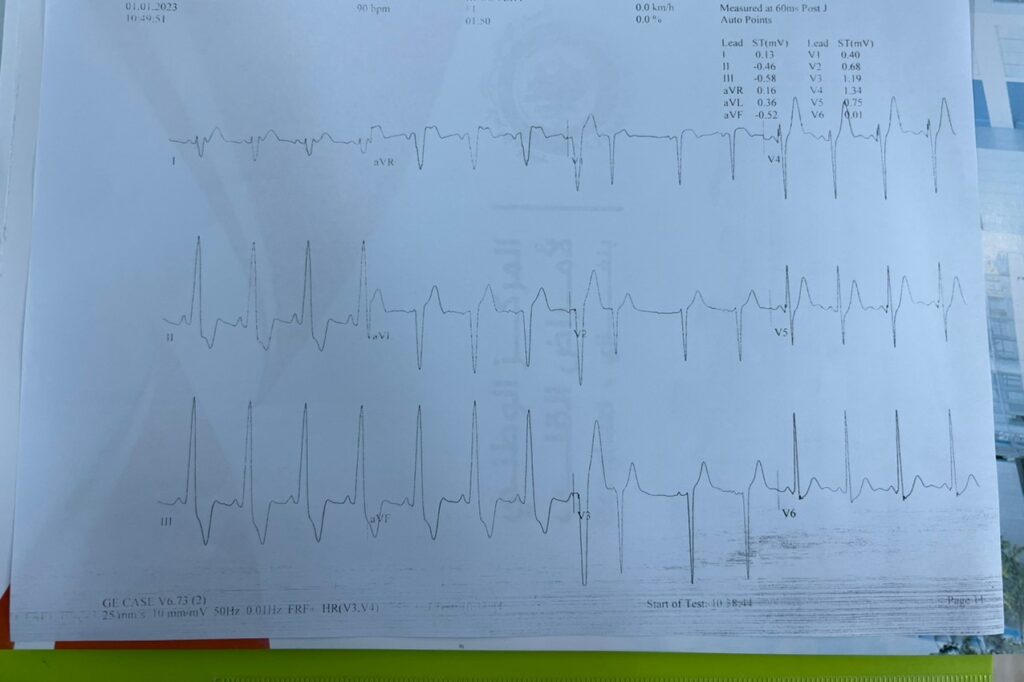
This was his ECG after the electrical cardioversion:
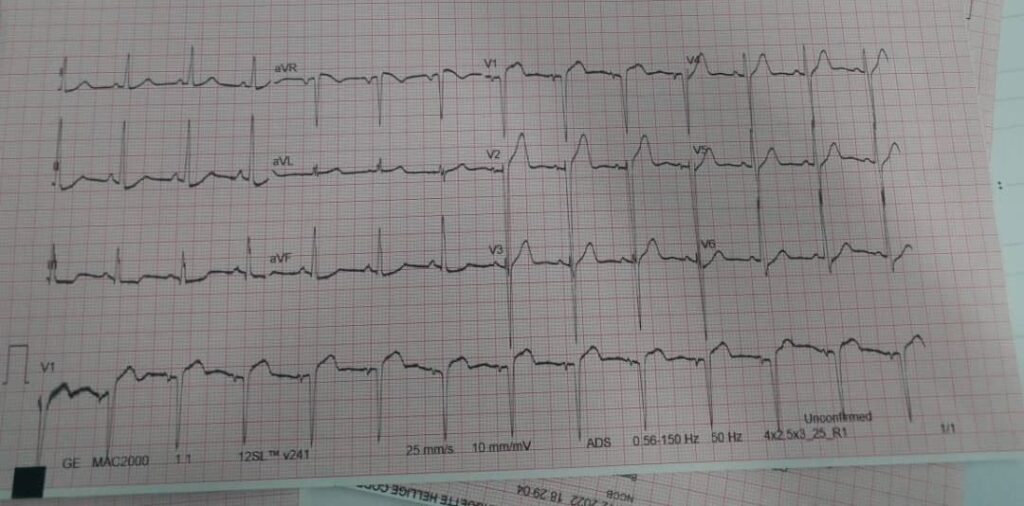
We can see that the patient has completely reverted to sinus rhythm, with a slight STE in leads V1 and V2 and STD in the inferior leads.. which could indicate an underlying ischemic process or Post-electrical cardioversion STE
Upon further discussion with the consultant on call, another diagnosis was risen up for discussion, the consultant cardiologist on call suspected that this was a case of Afib with aberrant conduction rather than a case of polymorphic VTACH..
Points in favor of Polymorphic VTACH:
- Wide complex tachycardia
- AV dissociation
- Capture beat – occur when the sinoatrial node transiently ‘captures’ the ventricles, in the midst of AV dissociation, to produce a QRS complex of normal duration
- Fusion Beat – occur when a sinus and ventricular beat coincide to produce a hybrid complex of intermediate morphology
Points in favor of AF with aberrant conduction:
- Irregular rhythm
- No change in the axis in both pre and post cardioversion which argue against VT
- Absence of RsR pattern in V1 (which is the most specific finding in favor of VT)
- His QT was not prolonged in post cardioversion ECG which argue against tDP
The wide QRS in AF with aberrant conduction is owed to one of two main things, an accessory pathway or it could be rate related

Also his CE were negative, but if they were positive there are two possibilities:
- Prolonged and sustained AF
- Faulty sample/lab technique
On the next day:
After further discussing the patient’s condition and taking a full history, as well as after checking the full labs of the patient, we decided to either 1) cath the patient (which was not available at the time) or 2) exercise the patient
This decision came about for two main reasons:
- To not label the patient as a case of VT without concrete proof (as he will need further management and even ICD insertion eventually)
- To make sure he gets the appropriate treatment if he was indeed a case of AF, he might need a lifelong anticoagulant therapy
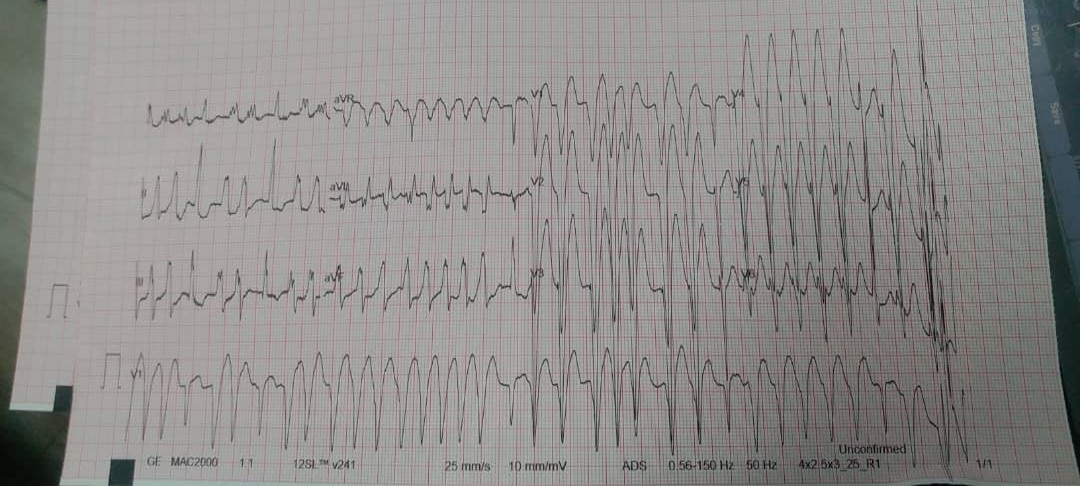
During the exercise test, the room was fully prepared with emergency management if the patient collapses. Upon starting the test, the patient ran through an almost complete exercise test with no problems at all, the changes in his rhythm throughout the stages are seen below:
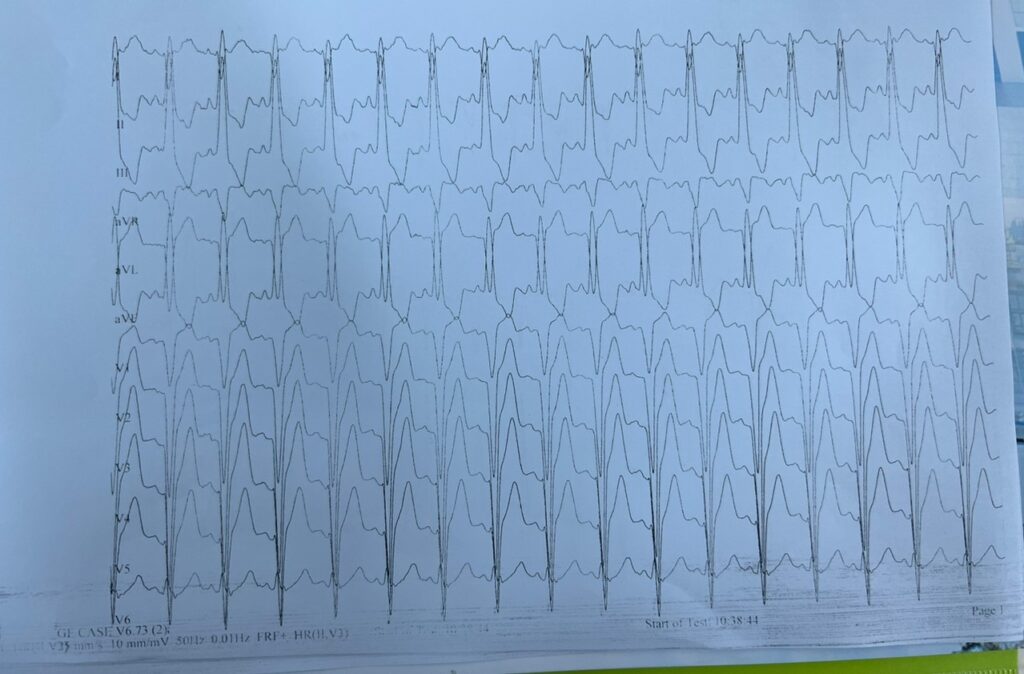
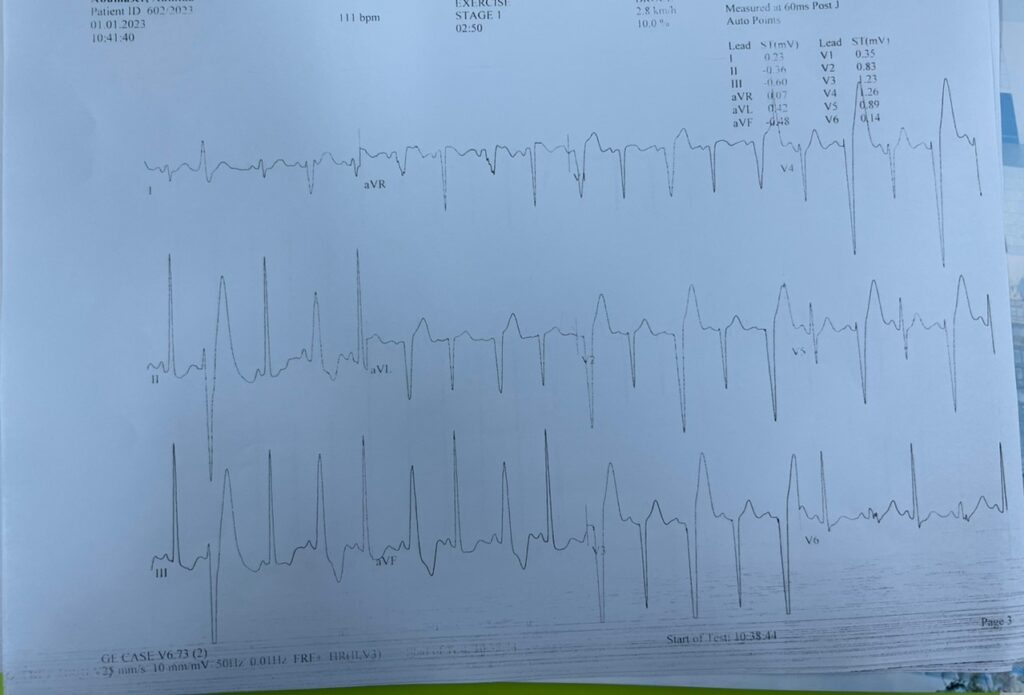
His exercise test demonstrated a pattern of rate-dependent LBBB.
The patient was discharged with a follow-up appointment in one week. Had the patient been labelled as a case of VT, he would have remained in the CCU for no reason, eventually contracting some nosocomial infection, and he definitely would have been labelled as a case of VT for the remainder of his life.
Takeaway message:
- As junior doctors it is easy to confuse some of the more complicated rhythms.
- Always consult your senior doctor before initiating thrombolysis or taking a grey decision.
- You have to be decisive in these crucial moments, and the best way to do so is by reinforcing your knowledge.
- You have to know the difference between AF with aberrant conduction and VT
- You have to know the exact doses of antiarrhythmic drugs and the manner by which they’re given e.g. Cordarone is given in 150mg bolus dose at a rate of 30mg/min MAX.
- You have to know which rhythms are shockable and which are not shockable.
Special thanks to:
- Dr. Jumaa Alfarsi (consultant cardiologist – head of unit B National Heart Center)
- Dr. Ali Rageb (specialist cardiologist – unit B National Heart Center)
- Dr. Amal Alwerfali – DOD that day (unit B National Heart Center)
Case written and edited by:
- Dr. Mohamed T. Shembesh (unit B National Heart Center)
Useful links:
- Everything you need to know about Amiodarone (Cordarone) – https://www.lhsc.on.ca/critical-care-trauma-centre/amiodarone-cordarone
- VT vs. AF with Aberrancy – http://www.emdocs.net/ecg-pointers-atrial-fibrillation-with-aberrancy/
No responses yet