Case presentation:
A 73 year old MLP, heavy smoker, k/c of COPD
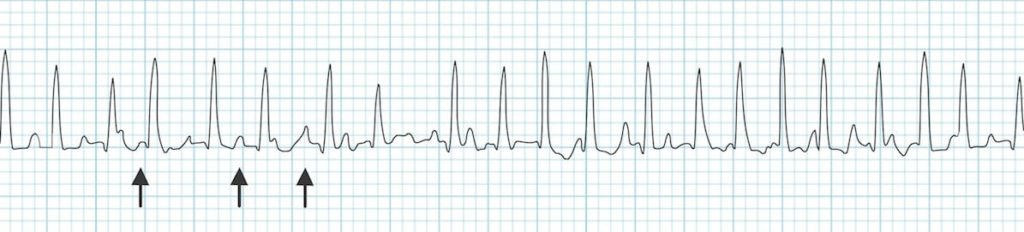
- Rapid irregular rhythm > 100 bpm.
- At least 3 distinctive P-wave morphologies (arrows).
Diagnosis: Multifocal Atrial Tachycardia
Multifocal Atrial Tachycardia (MAT)
- A rapid, irregular atrial rhythm arising from multiple ectopic foci within the atria.
- Most commonly seen in patients with severe COPD or congestive heart failure.
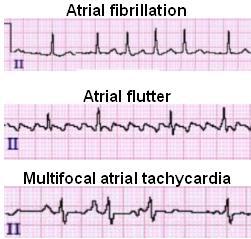
- It is typically a transitional rhythm between frequent premature atrial complexes (PACs) and atrial flutter / fibrillation.
AKA “Chaotic atrial tachycardia”
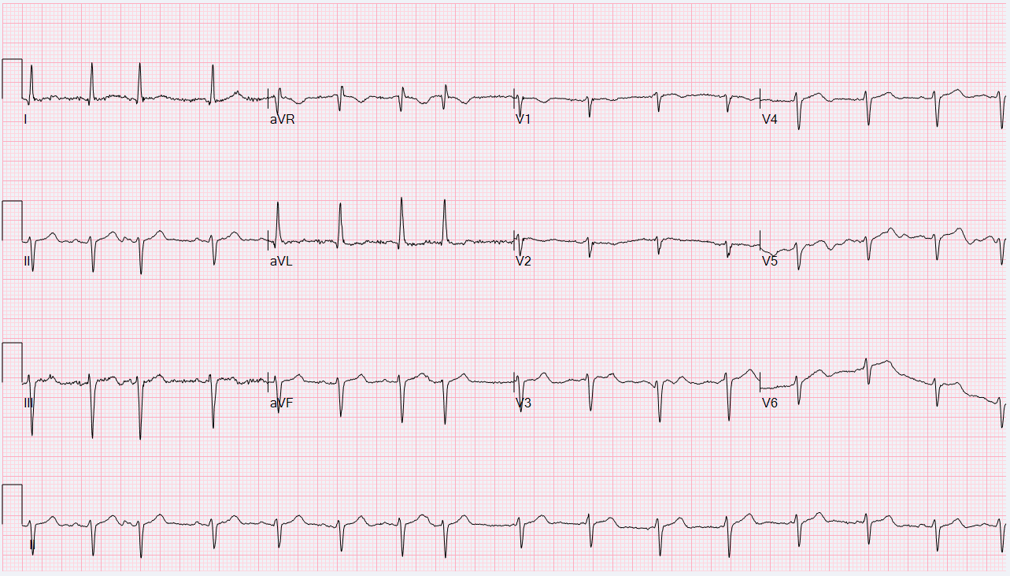
ECG Features
- Heart rate > 100 bpm (usually 100-150 bpm; may be as high as 250 bpm).
- Irregularly irregular rhythm with varying PP, PR and RR intervals.
- At least 3 distinct P-wave morphologies in the same lead.
- Isoelectric baseline between P-waves (i.e. no flutter waves).
- Absence of a single dominant atrial pacemaker (i.e. not just sinus rhythm with frequent PACs).
- Some P waves may be nonconducted; others may be aberrantly conducted to the ventricles.
There may be additional electrocardiographic features suggestive of COPD.
Clinical Relevance
- Usually occurs in seriously ill elderly patients with respiratory failure (e.g. exacerbation of COPD / CHF).
- Tends to resolve following treatment of the underlying disorder.
- The development of MAT during an acute illness is a poor prognostic sign, associated with a 60% in-hospital mortality and mean survival of just over a year. Death occurs due to the underlying illness; not the arrhythmia itself.
Mechanism
Arises due to a combination of factors that are present in hospitalised patients with acute-on-chronic respiratory failure:
- Right atrial dilatation (from cor pulmonale)
- Increased sympathetic drive
- Hypoxia and hypercarbia
- Beta-agonists
- Theophylline
- Electrolyte abnormalities: Hypokalaemia and hypomagnesaemia (e.g. secondary to diuretics / beta-agonists)
The net result is increased atrial automaticity.
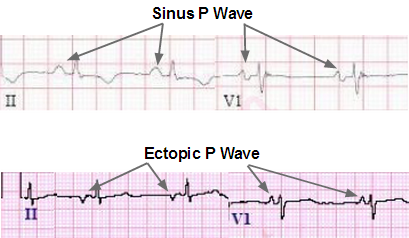
- Each QRS complex will be preceded by a P wave; however, each P wave will have a different morphology because they originate from different areas. By definition, multifocal atrial tachycardia must have at least three distinctly different P wave morphologies and a ventricular rate of greater than 100 beats per minute.
What if you saw an ECG with the same exact picture but the rate was <100bpm?
- Irregularly irregular
- Different P wave morphologies
- Irregularly irregular rhythm with varying PP, PR and RR intervals.
- Isoelectric baseline between P-waves
- Rate <100 bpm
Diagnosis: WAP (wandering atrial pacemaker)
Wandering Atrial Pacemaker (WAP)
Wandering atrial pacemaker is similar to multifocal atrial tachycardia except the heart rate is normal ― that is, less than 100 beats per minute.
Wandering atrial pacemaker occurs when multiple areas (ectopic foci) within the atrium generate consecutive action potentials that are all conducted to the ventricles. Thus, each QRS complex will be preceded by a P wave ― though each P wave will have a different morphology, as it is originating from a different area.
By definition, WAP must have at least three distinctly different P wave morphologies and a ventricular rate of less than 100 bpm.
P.S.
There is no thromboembolism risk in MAT, such as seen in atrial fibrillation or atrial flutter, as the atrium are contractile in MAT. If the heart rate is less than 100 beats per minute, then the rhythm is wandering atrial pacemaker, or WAP.
References:
- LITFL
- Healio
Special thanks to:
- Dr. Jumaa Alfarsi for explaining the concept in his Advanced ECG Course
No responses yet