A 48 years old MLP presented to the cardiac ER with chest pain and sweating, the chest pain was atypical (did not fulfil criteria of anginal pain e.g. not exacerbated on exertion, nor relived by rest or GTN), he is a known case of IHD with stent since 2019
On examination the patient looks unwell, dyspneic and sweaty
His BP was within normal range, his HR was around 180bpm, he said that he was completely well a few minutes prior to this episode, and he mentioned something about similar previous attacks
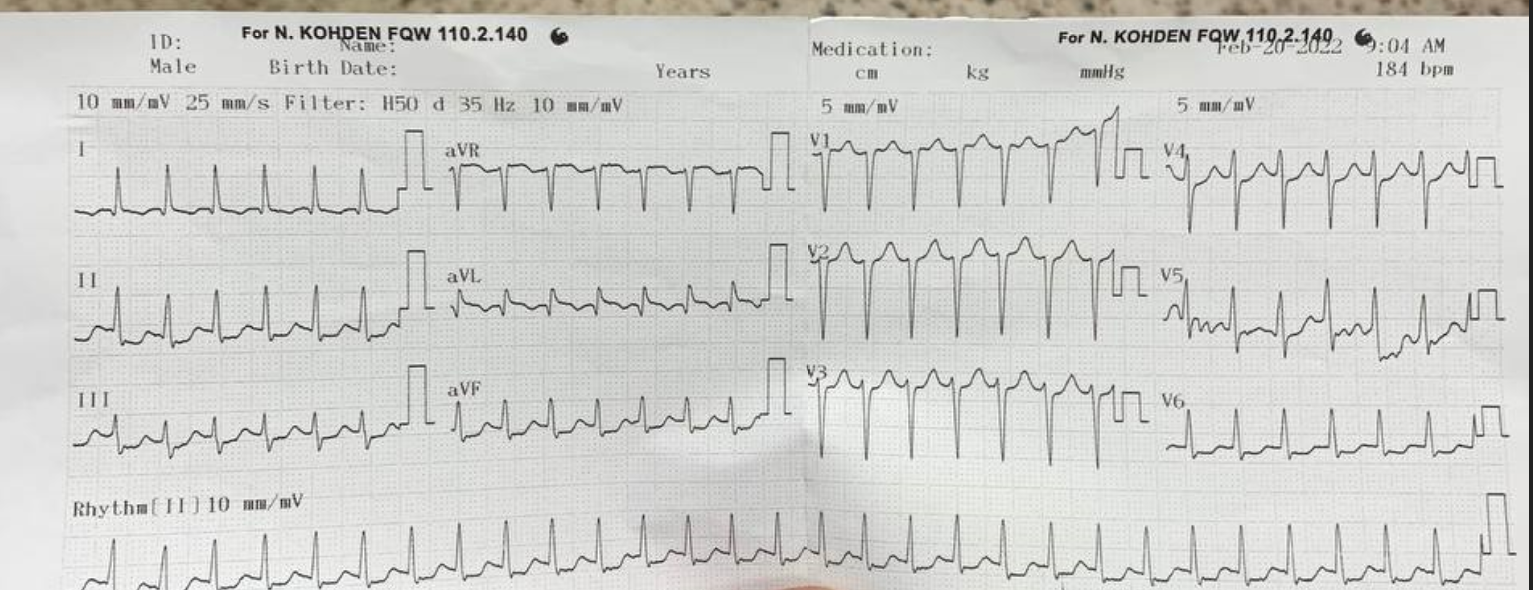
This is his ECG:
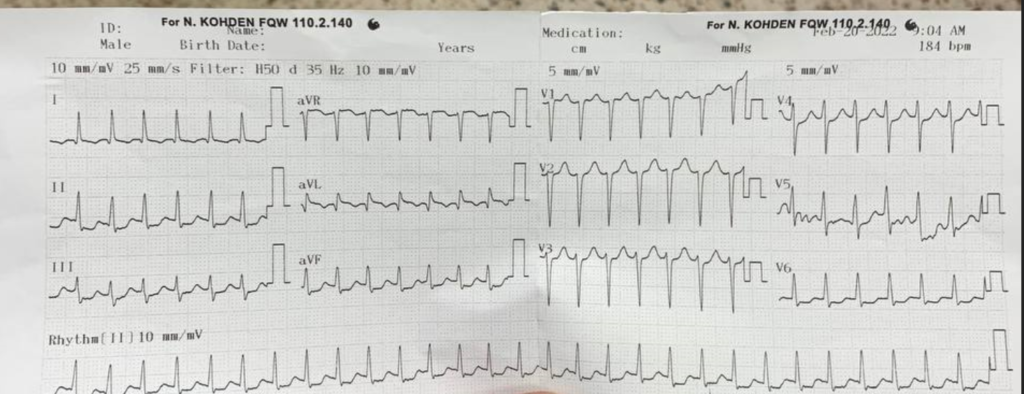
This ECG is characteristic of SVT (AVNRT) or pSVT aka paradoxical SVT.. It is very important to recognize this pattern as it is very common:
- Regular tachycardia ~140-280 bpm
- Narrow QRS complexes (< 120ms) unless there is co-existing bundle branch block, accessory pathway, or rate-related aberrant conduction
- P waves if visible exhibit retrograde conduction with P-wave inversion in leads II, III, aVF. They may be buried within, visible after, or very rarely visible before the QRS complex
We managed this patient with:
- Valsalva maneuvers (which did not yield any benefit in this case)
- Adenosine (first line medication in SVT) – we gave the patient 6 mg followed by rapid flush, observed for a few seconds, but the rate did not change so we gave another 12mg and observed, unfortunately the patient did not revert even then so we gave another 12mg adding up to the total allowed dose of 30mg
- Verapamil aka Isoptin – we gave the patient the first 5mg and observed for a few minutes, the patient immediately improved after the verapamil dose
In this situation we gave both Adenosine and Verapamil because the patient is a k/c of SVT and he had multiple episodes prior, he was always treated with the Verapamil but unfortunately it wasn’t available when the patient first arrived so we went for the Adenosine first, luckily his relative provided the Verapamil later on, and the patient responded without us having to DC shock him.
Generally when managing SVT (AVNRT), you should start with:
- Valsalva maneuver – a good portion of the patients improve by this alone
Then:
- Adenosine (6/12/12 total of 30mg) give the first 6mg rapidly followed by a 20cc flush of normal saline, observe for a few seconds and give the 12 then the last 12 as needed if the patient did not improve
OR
- Verapamil – an alternative to adenosine, which is given as 5/10/10 max dose of 25, give the first 5 mg and wait for 12-20 minutes then give the second 10mg, then if needed give the last 10mg
Last line:
- If neither the Valsalva nor the medications worked, the last line here is DC shock (synchronized electrical cardioversion) at 100-150J is usually sufficient
Further information about SVT:
The term supraventricular tachycardia (SVT) refers to any tachydysrhythmia arising from above the level of the Bundle of His, and encompasses regular atrial, irregular atrial, and regular atrioventricular tachycardias
- It is often used synonymously with AV nodal re-entry tachycardia (AVNRT), a form of SVT
- In the absence of aberrant conduction (e.g. bundle branch block), the ECG will demonstrate a narrow complex tachycardia
- Paroxysmal SVT (pSVT) describes an SVT with abrupt onset and offset – characteristically seen with re-entrant tachycardias involving the AV node such as AVNRT or atrioventricular re-entry tachycardia (AVRT)
Classification of SVT by site of origin and regularity
Regular Atrial
- Sinus tachycardia
- Atrial tachycardia
- Atrial flutter
- Inappropriate sinus tachycardia
- Sinus node reentrant tachycardia
Irregular Atrial
- Atrial fibrillation
- Atrial flutter (variable block)
- Multifocal atrial tachycardia
Regular Atrioventricular
- AVRT
- AVNRT
- Automatic junctional tachycardia
AV Nodal Re-entry Tachycardia (AVNRT)
- This is the commonest cause of palpitations in patients with structurally normal hearts
- AVNRT is typically paroxysmal and may occur spontaneously or upon provocation with exertion, caffeine, alcohol, beta-agonists (salbutamol) or sympathomimetics (amphetamines)
- It is more common in women than men (~ 75% of cases occurring in women) and may occur in young and healthy patients as well as those suffering chronic heart disease
- Patients will typically complain of the sudden onset of rapid, regular palpitations. Other associated symptoms may include:
- Presyncope or syncope due to a transient fall in blood pressure
- Chest pain, especially in the context of underlying coronary artery disease
- Dyspnoea
- Anxiety
- Rarely, polyuria due to elevated atrial pressures causing release of atrial natriuretic peptide
- The tachycardia typically ranges between 140-280 bpm and is regular in nature. It may self-resolve or continue indefinitely until medical treatment is sought
- The condition is generally well tolerated and is rarely life threatening in patients with pre-existing heart disease
Source:
- Patient was managed in NHC – Benghazi
- Further information about SVT from LITFL
No responses yet